The World Health Organization defines a fall as “an involuntary event resulting to a rest on the ground, floor or other lower level”. There are many factors contributing to a fall, including intrinsic causes such as patient’s age, physiological and psychological state, medical history, as well as extrinsic causes such as poor lighting, wet floor, floor has obstacles, inappropriate footwear and inappropriate mobility aid.
The undesirable consequences from a fall may lead to physical injuries such as bruising, fractures as well as psychological and social effects. This is known as the ‘post-fall syndrome’, which is the constant fear of a repeated fall, and may cause the victim to disengage in daily activities and thus affecting their quality of life.
In KTPH, we have implemented a comprehensive falls assessment, intervention and education program. Some of these measures include identifying patients as high risk using bright green wrist tags and good practices such as regularly addressing patients’ personal and toileting needs and incorporating safety features in the design of our environment. Physiotherapists and Occupational Therapists including other allied health professionals are an integral part of the multidisciplinary team who contribute to risk assessment and falls prevention program in the hospital and maintain functional independence.
Family members and caregivers are educated on falls risk prevention and they are encouraged to follow safe behavioural practices such as putting up cot sides and informing the nurses prior to leaving after visiting. The family members are also encouraged to accompany confused and restless patients during their stay in the hospital.
Annual Falls Awareness Day is held to engage public in understanding the falls risk and prevention measures, and provide necessary resources available in the community to reduce falls in the community.
From January 2022 to December 2022, the average incidence was 1.03 inpatient falls per 1000 patient days, which is comparable when benchmarked with the national falls prevention indicators (National average of 0.90 falls per 1,000 patient days in 2020)
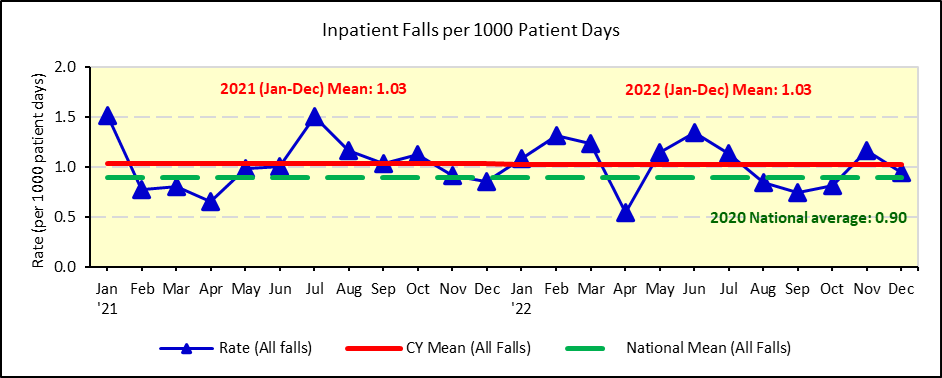 Figure 1: Incidence of Inpatient Falls per 1,000 patient days
Figure 1: Incidence of Inpatient Falls per 1,000 patient days
From January 2022 to December 2022, the average incidence was 0.03 inpatient falls with major injury per 1000 patient days.
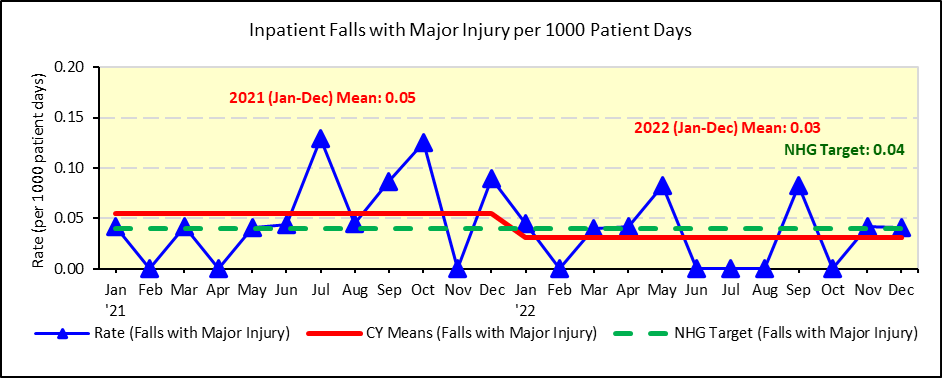 Figure 2: Incidence of Inpatient Falls with Major Injury per 1,000 patient days
Figure 2: Incidence of Inpatient Falls with Major Injury per 1,000 patient days
References:
- How do you measure fall rates and fall prevention practices? January 2013. Agency for Healthcare Research and Quality, Rockville, MD. National Database of Nursing Quality Indicator (NDNQI)
- World Health Organization, Media centre, Falls, Fact sheet, reviewed Jan 2018.
- Ministry of Health, Singapore, NSHC Self-Assessment Indicators for Public Hospitals and Institutions, 2018
